More on focused shockwave therapy...
Focused shock wave therapy for pain-free daily activity.
The group of musculoskeletal discorders we frequently use for both radial and focused shockwave therapy are: plantarfasciosis, achilles tendinosis, patella tendinosis (runners knee), greater trochanteric pain syndrome, rotator cuff pain syndrome and both medial and lateral epicondylosis (golfers and tennis elbow). The conditions we are better off treating with focused shockwave are: greater trochanteric pain syndrome, any of the aforementioned conditions involving enthesopathy (insertional tendinosis), calcific tendinopathies, non-union of fracture and in cases where radial shockwave is too painful to use.
These conditions lead to discomfort and limitations in everyday activities that negatively affect quality of life and mental well-being [1]. Pain and associated stress can prolong the healing process.
A meta-analysis by Schmitz et al. concluded that extracorporeal shock wave therapy is an effective, safe and non-invasive treatment option for patients with musculoskeletal disorders [2]. It does not involve any medications or injections. As such, it is worth emphasizing that focused shock wave therapy can be used as an alternative to more invasive treatments such as cortisone injections or orthopedic surgery. It can also be used as an alternative to pain killers and other therapeutic options with potentially severe side effects. Our Focused Shockwave device enables the treatment of pathologies located up to 12 cm deep in the skin. This unique capability allows us to treat deep and calcified musculoskeletal lesions, trigger points, myofascial pain syndrome, nonunion fractures and enthesopathies resistant to healing.
A review of the PEDro (Physiotherapy Evidence Database) – the reference database for randomized clinical trials (RCTs), systematic reviews and clinical practice guidelines in the field of physiotherapy – indicates that 66 RCTs (out of 81) using Focused Shock Waves Therapy resulted in statistically significant positive outcomes for patients [3].
Below is a selection of the most notable effects achieved with FSWT. A study by Rompe et al. [4] on the impact of focused extracorporeal shock wave therapy (FSWT) and local anesthesia on treatment of plantar fasciopathy found that:
- a significantly greater number of patients treated exclusively with focused shock waves achieved a more than 50% reduction in pain at 3 months follow-up compared to patients receiving combined therapy with local anesthesia (67% FSWT only vs. 29% FSWT + local anesthesia). Studies by Lee et al. [5], Kim et al. [6] and Chen et al.
- [7] demonstrated the utility of FSWT in disabling pain due to knee osteoarthritis with a combination of FSWT and conservative physical therapy resulted in better clinical outcomes than conservative physical therapy alone. Patients reported a significant improvement in the range of motion of the knee joint.
Data published by Cacchio et al. [8] demonstrated the utility of FSWT in patients with hypertrophic long-bone nonunions:
- reduction in pain without adverse side effects;
- safe and efficient – a positive energy flux density of 0.4 mJ/mm2 appears to be sufficient for this indication;
- clinicians should opt for fESWT over surgery in the management of hypertrophic long-bone nonunions.
Therapeutic shock waves: the sound of healing – but how are they created?
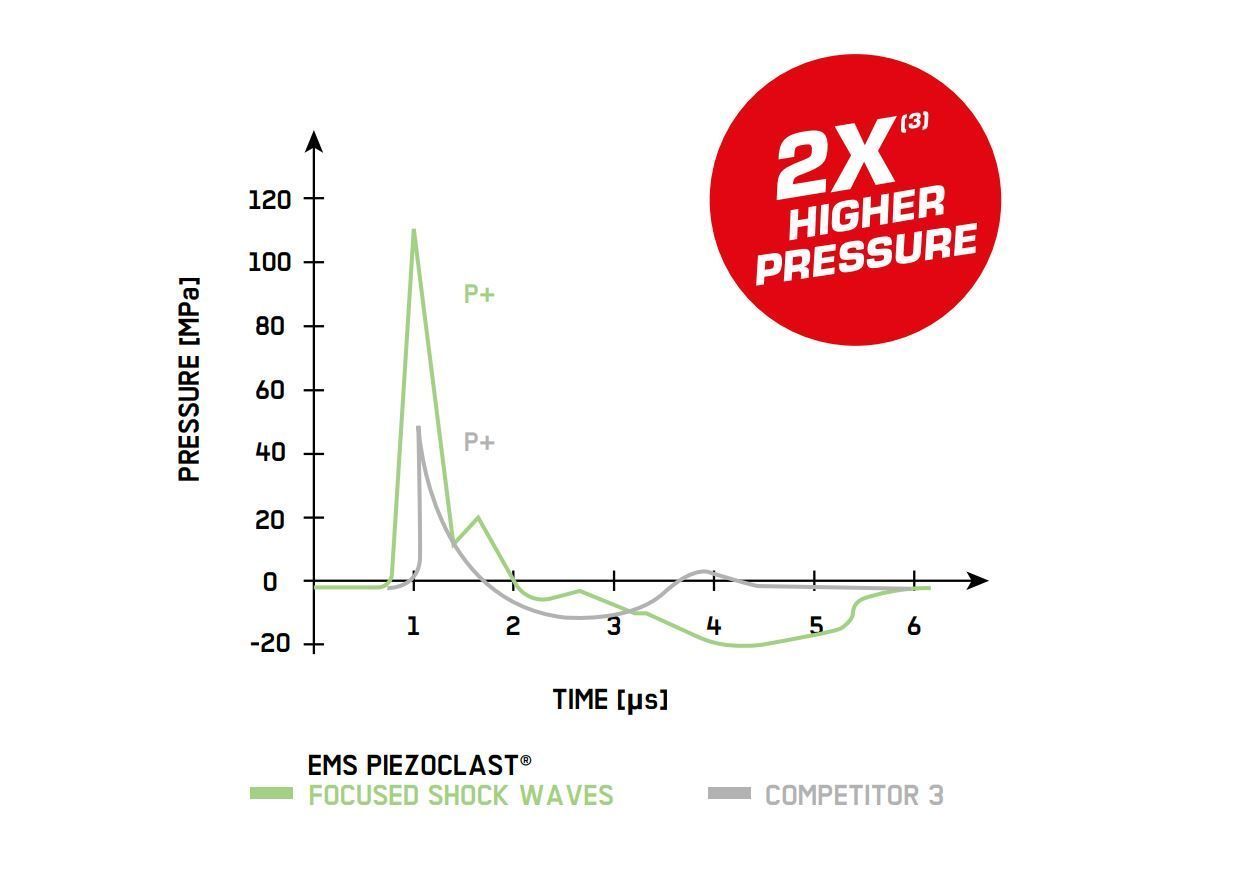
Let’s start with some basic definitions: shock waves are mechanical acoustic waves characterized by propagating disturbance that moves faster than the local speed of sound in the medium [9]. It is associated with a sudden rise from ambient pressure to its maximum pressure. In general, extracorporeal shock waves are characterized by the development of pressure over time.
How do focused extracorporeal shock waves act on the musculoskeletal system?
Extracorporeal shock waves are known to generate cavitation within the treated area [10]. Cavitation means the rapid formation, expansion, and forceful collapse of gas bubbles in liquids and is associated with rapid pressure changes [11]. Cavitation plays an important role in mediating the molecular and cellular mechanisms of action within the musculoskeletal system [10].
The DolorClast® Focused Shock Waves device uses piezoelectric technology. In simple terms, this means that a large number of piezocrystals are contained in the bowl-shaped handpiece. When rapid electrical discharge is applied, these thousands of piezocrystals react with a pattern of deformation (contraction and expansion). This is known as the piezoelectric effect: when electricity is passed through the crystals, they ‘squeeze themselves’ by vibrating back and forth. Piezoelectricity (or the piezoelectric effect) is the appearance of an electrical potential (i.e. a voltage) across the sides of a crystal when it is subjected to mechanical stress (i.e. squeezed). This induces an acoustic pressure pulse in the surrounding environment that can steep into a shock wave. When focused shock waves are generated using piezoceramic materials, this avoids mechanical displacement of the handpiece on the skin and prevents the need for treatment to occur under excessive pressure. The end result is that shock waves are focused and dispersed within the tissues. This highlights another important feature of DolorClast® Focused Shock Waves: that they can be used in patients with low pain thresholds.
How is the sensation of pain generated in the human body?
First, it is detected as sensory information by nociceptors located on free nerve endings; then, it is carried via A-delta and group C nerve fibers from the periphery to the dorsal horn of the spinal cord. This transmission of pain information is mediated by a number of neurotransmitters. Here, we will focus on one of them: substance P [12]. During shockwave therapy, an increased level of substance P [12] is also what is responsible for any discomfort or unpleasant sensations. Substance P and other neuropeptides are released from the peripheral ends of sensory nerve fibers and result in a slight sensation of pain [13]. Herein lies the answer! The longer the C-fibers are activated with shockwaves, the lower the concentration of substance P within the treated area. As a result, the nociceptors are no longer sufficiently stimulated. Less substance P in the tissue leads to pain relief (because the transmission between injury and brain is ineffective) and inhibits the neurogenic inflammation process [12, 14].
This effect can be explained in layman’s terms using the example of red chili peppers, which contain capsaicin. At first, the substance overwhelms the C-nerve fibers responsible for the sensation of burning in the mouth. However, after a couple of minutes, the feeling disappears and the tongue becomes numb. Anyone who has ever tried hot peppers should be familiar with this experience! Shock waves act on the musculoskeletal system via a number of molecular and cellular mechanisms.
- They lower the substance P concentration and bring about pain relief.
- They block the neurogenic inflammation process that plays an important role in the pathogenesis of tendinopathies (such as tennis elbow or plantar fasciopathy).
- They activate the formation of primary muscle cells (to repair damaged muscle fibers) and increase expression of the following growth factors:
VEGF (Vascular Endothelial Growth Factor), which plays an important role in angiogenesis. It promotes the formation of new blood vessels and accelerates tissue healing [15,16,17,18],
PCNA (Proliferating Cell Nuclear Antigen) and eNOS (Endothelial Nitric Oxide Synthase), which are the growth factors responsible for stimulating blood circulation. An improved flow of oxygenated blood promotes tissue regeneration [15,19,20,21].
| Tendons | Cartlidge | Bone |
|---|---|---|
| Stimulate tendon remodeling [22] | Promote the proliferation and self-renewal of mesenchymal stem cells, which prevent cartilage from degrading and accelerate the cartilage repair process [24,25] | Up-regulate the expression of BMP (Bone Morphogenetic Protein), a growth factor that stimulates bone healing [24,25,27] |
| Increase the expression of lubricin in the synovial joint, which is responsible for coating the cartilage surface. This, in turn, facilitates tendon gliding and decreases erosive wear [23 | Increase the expression of primary osteoblasts, thus promoting new bone formation [28,29,30] | |
| Examples of indications | for each mechanism | of action: |
| Plantar fasciopathy, Achilles tendinopathy | Knee osteoarthritis | Nonunion fractures |
We rely on clinical evidence!
References:
1. https://www.who.int/news-room/fact-sheets/detail/musculoskeletal-conditions
2. Yang, Tsung-Hsun et al. “Efficacy of Radial Extracorporeal Shock Wave Therapy on Lateral Epicondylosis, and Changes in the Common Extensor Tendon Stiffness with Pretherapy and Posttherapy in Real-Time Sonoelastography: A Randomized Controlled Study.” American journal of physical medicine & rehabilitation vol. 96,2 (2017): 93-100.
3. Schmitz, Christoph et al. “Efficacy and safety of extracorporeal shock wave therapy for orthopedic conditions: a systematic review on studies listed in the PEDro database.” British medical bulletin vol. 116,1 (2015): 115-38
4. Rompe JD, Meurer A, Nafe B, Hofmann A, Gerdesmeyer L. Repetitive low-energy shock wave application without local anesthesia is more efficient than repetitive low-energy shock wave application with local anesthesia in the treatment of chronic plantar fasciitis. J Orthop Res 2005;23:931-941.
5. Lee JH, Lee S, Choi S, Choi YH, Lee K. The effects of extracorporeal shock wave therapy on the pain and function of patients with degenerative knee arthritis. J Phys Ther Sci 2017;29:536-538.
6. Kim JH, Kim JY, Choi CM, Lee JK, Kee HS, Jung KI, Yoon SR. The dose-related effects of extracorporeal shock wave therapy for knee osteoarthritis. Ann Rehabil Med 2015;39:616-623.
7. Chen, Tien-Wen et al. “The efficacy of shock wave therapy in patients with knee osteoarthritis and popliteal cyamella.” The Kaohsiung journal of medical sciences vol. 30,7 (2014): 362-70.
8. Cacchio A, Giordano L, Colafarina O, Rompe JD, Tavernese E, Ioppolo F, et al. Extracorporeal shock-wave therapy compared with surgery for hypertrophic long-bone nonunions. J Bone Joint Surg Am 2009;
91:2589-2597 9. Zel’Dovich, Y. B., & Raizer, Y. P. (2012). Physics of shock waves and high-temperature hydrodynamic phenomena. Courier Corporation.
10. Ogden, J A et al. “Principles of shock wave therapy.” Clinical orthopaedics and related research ,387 (2001): 8-17.
11. Schmitz C, Császár NBM, Rompe JD, Chaves H, Furia JP. Treatment of chronic plantar fasciopathy with extracorporeal shock waves (review). J Orthop Surg Res. 2013; 8: 31.
12. Maier M, Averbeck B, Milz S, Refior HJ, Schmitz C. Substance P and prostaglandin E2 release after shock wave application to the rabbit femur. Clin Orthop Relat Res. 2003;(406):237-245.
13. Juránek I, Lembeck F. Afferent C-fibres release substance P and glutamate. Can J Physiol Pharmacol. 1997 Jun;75(6):661-4.
14. Hausdorf J, Lemmens MA, Kaplan S, et al. Extracorporeal shockwave application to the distal femur of rabbits diminishes the number of neurons immunoreactive for substance P in dorsal root ganglia L5. Brain Res. 2008;1207:96-101.
15. Kuo YR, Wang CT, Wang FS, Chiang YC, Wang CJ. Extracorporeal shock-wave therapy enhanced wound healing via increasing topical blood perfusion and tissue regeneration in a rat model of STZ-induced diabetes. Wound Repair Regen. 2009;17(4):522-530.
16. Meirer R, Brunner A, Deibl M, Oehlbauer M, Piza-Katzer H, Kamelger FS. Shock wave therapy reduces necrotic flap zones and induces VEGF expression in animal epigastric skin flap model. J Reconstr Microsurg. 2007;23(4):231-236.
17. Stojadinovic A, Elster EA, Anam K, et al. Angiogenic response to extracorporeal shock wave treatment in murine skin isografts. Angiogenesis. 2008;11(4):369-380.
18. Yan X, Zeng B, Chai Y, Luo C, Li X. Improvement of blood flow, expression of nitric oxide, and vascular endothelial growth factor by low-energy shockwave therapy in random-pattern skin flap model. Ann Plast Surg. 2008;61(6):646-653.
19. Calcagni M, Chen F, Högger DC, et al. Microvascular response to shock wave application in striated skin muscle. J Surg Res. 2011;171(1):347-354.
20. Contaldo C, Högger DC, Khorrami Borozadi M, et al. Radial pressure waves mediate apoptosis and functional angiogenesis during wound repair in ApoE deficient mice. Microvasc Res. 2012;84(1):24-33.
21. Kisch T, Wuerfel W, Forstmeier V, et al. Repetitive shock wave therapy improves muscular microcirculation. J Surg Res. 2016;201(2):440-445
22. Waugh CM, Morrissey D, Jones E, Riley GP, Langberg H, Screen HR. In vivo biological response to extracorporeal shockwave therapy in human tendinopathy. Eur Cell Mater. 2015;29:268-280.
23. Zhang D, Kearney CJ, Cheriyan T, Schmid TM, Spector M. Extracorporeal shockwave-induced expression of lubricin in tendons and septa. Cell Tissue Res. 2011;346(2):255-262.
24. Wang CJ, Sun YC, Wong T, Hsu SL, Chou WY, Chang HW. Extracorporeal shockwave therapy shows time-dependent chondroprotective effects in osteoarthritis of the knee in rats. J Surg Res. 2012;178(1):196-205.
25. Zhang H, Li ZL, Yang F, et al. Radial shockwave treatment promotes human mesenchymal stem cell self-renewal and enhances cartilage healing. Stem Cell Res Ther. 2018;9(1):54.
26. Wang CJ, Wang FS, Yang KD. Biological effects of extracorporeal shockwave in bone healing: a study in rabbits. Arch Orthop Trauma Surg. 2008;128(8):879
27. Wang CJ, Yang KD, Ko JY, Huang CC, Huang HY, Wang FS. The effects of shockwave on bone healing and systemic concentrations of nitric oxide (NO), TGF-beta1, VEGF and BMP-2 in long bone non-unions. Nitric Oxide. 2009;20(4):298-303.
28. Gollwitzer H, Gloeck T, Roessner M, et al. Radial extracorporeal shock wave therapy (rESWT) induces new bone formation in vivo: results of an animal study in rabbits. Ultrasound Med Biol. 2013;39(1):126-133.
29. Hofmann A, Ritz U, Hessmann MH, Alini M, Rommens PM, Rompe JD. Extracorporeal shock wave-mediated changes in proliferation, differentiation, and gene expression of human osteoblasts. J Trauma. 2008;65(6):1402-1410.
30. Tischer T, Milz S, Weiler C, et al. Dose-dependent new bone formation by extracorporeal shock wave application on the intact femur of rabbits. Eur Surg Res. 2008;41(1):44-53.
31. Katharina Sternecker et al., Exposure of zebra mussels to extracorporeal shock waves demonstrates formation of new mineralized tissue inside and outside the focus zone. Biology Open 2018;
32. Perez et al., Acoustic field characterization of the Duolith: Measurements and modeling of a clinical shock wave therapy device. J Acoust Soc Am. 2013 Aug; 134(2): 1663–1674.