Headaches
TENSION TYPE HEADACHES
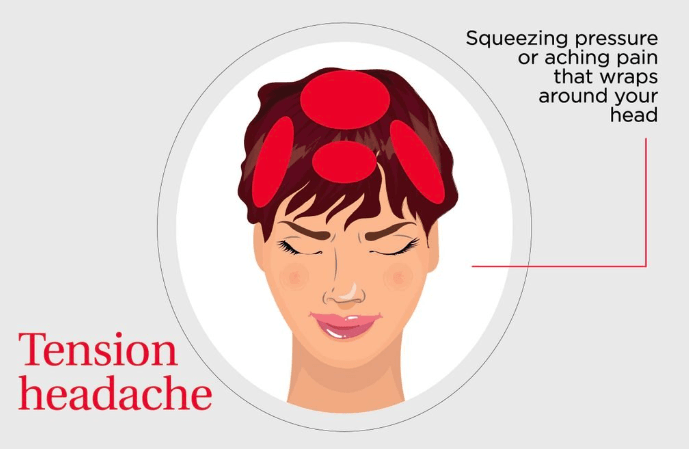
Tension Type is considered the most common type of headache. They are often mild to moderate in severity, can last from 30 minutes up to 7 days and mostly felt on either side of the head. People often describe it like they are wearing a tight band or hat around their head.
STRESS is a major contributing factor for these types of headaches and that’s why most of us will experience one at some stage in our lives.
The exact cause is not fully understood and certain neurobiological processes are thought to be involved but until we know more, keep an eye out for these common triggers:
- Stress, anxiety and depression
- Poor posture
- Bright and noisy environments
- Eye strain (from prolonged periods of screen time)
- Smoking
- Caffeine dependence/withdrawal
- Dehydration
Tension headaches are unlikely to make you feel nauseous or make you vomit and they do not present with an ‘aura’ (a distinguishing feature of migraines).
You may experience them frequently enough that they become a chronic condition for you where it can really start to affect your personal, professional and social life.
It cannot be stressed enough (pun intended) that lifestyle changes and stress-minimising behaviours are key components to any management plan for tension type headaches and should be discussed with your healthcare professional. There are pharmaceutical options and your General Practitioner can discuss preventative medications with you to determine if this is an appropriate course of action.
Cervicogenic Headache
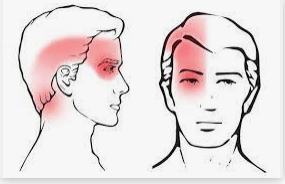
Let's break that word down. ‘Cervico’ essentially refers to the cervical spine. These are the vertebrae of your neck. And we can think of the word ‘genic’ as ‘generated from’. So to put it simply, this type of headache comes from the neck in one way or another.
These headaches are commonly felt in a ‘rams horn’ distribution and can be either unilateral or bilateral. These are usually associated with neck pain or dysfunction and may or may not be made worse with movement of the neck.
The upper cervical spine has a complex anatomical structure, with the muscles and joints playing an important role, supported by some pretty unique electrical wiring. A cervicogenic headache is thought to be a referred pain coming from the structures that are innervated by this neurological wiring. These structures include the cervical spinal joints, ligaments, discs and musculature.
It gets even more neuroanatomically complex but for now let's just look out for headaches that resemble the picture below and speak to your healthcare provider if you think you may be suffering from a cervicogenic headache.
Migraines
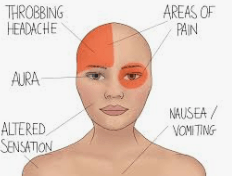
Let's start off with some statistics. Over 5 million Australians live with migraine, affecting 1 in 10 men and 1 in 3 women. Working-age women are the most significantly affected, with up to 45% of women aged between 25 and 45 experiencing migraine attacks. A migraine attack can last for days, weeks or even months.
Migraines are a complex and not-yet-fully-understood neurological condition that can cause debilitating headaches with a few other symptoms thrown on top. While migraine attacks can manifest and affect people in different ways within the scope of head pain, they are typically felt as a moderate to intense throbbing, pulsating or bounding pain on one side of the head. These can be aggravated by movement.
One of the following symptoms is usually present: nausea, vomiting, sensitivity to light (photophobia) and or sensitivity to sound (phonophobia).
While there is currently no cure for migraines, there are medical treatments and lifestyle changes that can make the condition manageable.
Migraines can be as unique as the person who suffers them, so it is important for your practitioner to be aware of the many signs and symptoms that can accompany a migraine. Some of these include:
- Aura (can include bright lights, zig zag lines or spots in the visual field)
- Confusion and difficulty concentrating
- Problems with speaking and coordination
- Stiffness in the neck and shoulders
- Other neurological symptoms like pins and needles, tingling or even limb weakness
- Vertigo, nausea, vomiting
It is important to note that these symptoms can be very similar to things we may see in the more concerning types of headaches, that’s why it is always important to have any head pain you may be experiencing checked out by your healthcare provider.
Triggers are also an important facet of migraines to consider. Triggers are as individual as the migraine itself and what sets off your migraine may not impact another migraine sufferer at all.
As stated, triggers vary. Some have even claimed that changes in barometric pressure can set off their migraine.
The following are just some examples of triggers that you may experience:
- Brights lights or loud noises
- Changes in weather or temperatures
- Dehydration
- Emotional changes, stressful periods
- Hormonal changes
- Certain alcohol like red wine or foods like chocolate or cheese
- Changes in sleep patterns - associated with travel or shift work
- Skipping meals
Medical treatments for migraines include prophylactic or preventative medication, all of which would have to be discussed with your General Practitioner.
HOW CAN WE HELP!

Your Osteopath will focus on several areas to help manage your headache and migraines. These areas of the body may include the neck, the jaw, shoulders, upper back/thoracic spine and ribs. Practitioners employ a range of techniques which may include, but not limited to:
- Soft tissue techniques
- Muscle energy techniques
- Articulation/mobilisation of joints
- Joint manipulation (people know this more commonly as cracking joints)
- Stretching
- Rehabilitation
There are several aims of Osteopathic management, all of which your Osteopath will discuss with you, but this can include improving your general mobility in the areas addressed, reducing muscular tension/pressure on nerves and inflammation, advice to help prevent recurrence and address other aspects of your general lifestyle if needed.
References
- https://headacheaustralia.org.au/
- https://whatisosteo.com/body-map/head/headaches-and-migraine-explained/
- https://www.osteopathy.org.au/about-osteopathy/patient-information